Many patients do not know how to understand that you have osteonecrosis, but at the same time they are happy to have such a diagnosis for themselves. Meanwhile, the causes of back, lower back or neck pain can be many. It could be curvature of the spine, disruption of internal organs, tumor, infection, position of unstable vertebral bodies, etc. v. Therefore, you should not self-diagnose. Seek medical attention in case of pain.
There is no reliable algorithm for how to recognize osteonecrosis without special examination. But there are certain clinical signs that make this disease suspicious. We will talk about them in the material that interests you. In the meantime, we recommend that you familiarize yourself with the development mechanism of osteonecrosis.
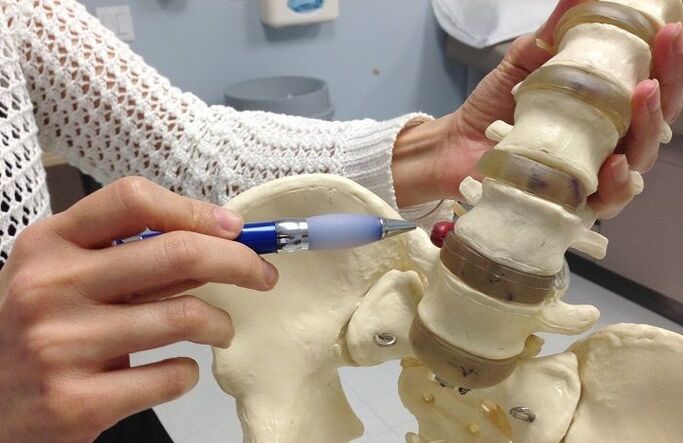
Degenerative dystrophy of the cartilage tissue of the disc - this is a pathology scientifically called osteonecrosis. As it develops, it leads to back pathology, complicated by back pain, sciatica, sciatica, sciatica, low back pain and other syndromes associated with damage to other tissues. together.
Osteoma is the result of maintaining a wrong lifestyle of a person. The contributing factors are:
- excess body weight - each kilogram creates an additional depreciation and mechanical load on the cartilage tissue of the intervertebral disc;
- sedentary lifestyle, no regular exercise for the musculature of the back;
- eat a large amount of carbohydrates, refined foods;
- wearing tight, uncomfortable clothes and shoes;
- improper posture, habit of stooping, stooping, leaning in one direction or another;
- incorrect placement of the foot in the form of a flatfoot or clubfoot;
- curvature of the spine;
- sedentary or hard labor;
- smoking and drinking alcoholic beverages;
- Not drinking enough clean water during the day.
All these factors slow down the microcirculation of blood in the capillary network in the thickness of muscle tissue. It turns out that it is not possible to carry out formal diffusion exchange with the cartilage tissues of the disc. They do not have their own circulatory system. This is how the mechanism of destruction of the capsule surface (this is the outer sheath of the disc) is triggered. It forms a deposit of calcium salts. They prevent the reception of fluids from the outside. Thus, the annulus begins to draw fluid from the nucleus pulposus within it. This colloid is responsible for maintaining the normal height and shape of the disc. Therefore, when fluid is lost, the pulp nucleus loses its ability to maintain the height of the disc. The second stage of osteonecrosis develops - protrusion of the eye.
In the third stage, the annulus ruptures and part of the nucleus pulposus prolapses. This is a herniated disc disease. It presses on the surrounding soft tissues, causing an inflammatory response, etc. v.
The fourth stage of osteonecrosis is the formation of a herniated disc mass. Part of the nucleus pulposus detaches or exits completely due to rupture of the annulus. If the herniated mass enters the cavity of the spinal canal, its release requires an emergency surgery. Otherwise, a person may remain disabled from physical paralysis for the rest of his or her life.
As you can see, this is a very serious disease that needs to be diagnosed promptly. The sooner complex treatment is started, the better the chance of fully restoring the integrity of the disc and its functions.
When the first signs of osteonecrosis appear, you can make an appointment with a chiropractor or neurologist. The doctor will conduct a manual examination and examination. They will make an accurate diagnosis and recommend necessary additional tests. After an accurate diagnosis, you will be given a course of treatment.
How to recognize cervical osteonecrosis?
How to understand that you have cervical osteonecrosis and not myositis, and what to do next? Before identifying cervical osteonecrosis, you need to collect a history of:
- when pain occurs;
- what actions provoke their appearance;
- how long ago the first seizure was;
- Are there any additional clinical signs?
- how the place to sleep and work is organized;
- what bad habits do you have;
- workplace and occupation.
How to understand that cervical osteonecrosis follows all this information? First of all, it should be known that degenerative disc disease manifests itself in the form of pain, stiffness when moving, and muscle tension in the neck and neck area only in the early stages. Then, tension headaches, dizziness, hearing and vision impairment, increased fatigue, decreased mental performance, etc. v. added to these markers.
A distinctive feature of cervical osteochondrosis is that exacerbation of symptoms begins at the end of the working day. And the patient's occupational activity is in most cases associated with prolonged static tension of the neck and collar muscles. On examination, there is pain on palpation of the vertebrae, excessive muscle tension, and increased pain when attempting to turn the head.
Before recognizing fibroids in the neck, the doctor recommends that the patient go for an X-ray. It shows reduced spaces between the vertebral bodies. This indicates that a convex is developing. With the help of X-ray imaging, an experienced spine specialist will be able to rule out instability in the position of the vertebral bodies, their exit, the healing process, thedegenerative joint process, destroy disc joints and a number of other serious diseases. If this test is not enough, then you should have an MRI or CT scan. If you suspect the development of posterior vertebral artery syndrome, you should conduct an ultrasound of the blood vessels of the neck and head.
How to recognize bone necrosis in the chest area
Before recognizing thoracic osteosarcoma, it is necessary to exclude the possibility of pathological development of internal organs, such as the heart, coronary circulatory system, lungs, pleura, bronchi, etc. v. Consider how to recognize thoracic osteonecrosis:
- the most important diagnostic technique is palpation, if the pain is determined only by torsion processes of the vertebrae and in the vertebral muscle region, then degenerative destruction of the cartilage tissue of the disc is not excluded;
- limited mobility and any turning and tilting of the body increases pain;
- pain caused by exertion, hypothermia, or psychological stressors;
- Deep breathing does not make the pain worse.
It is very important to understand cardiac or osteonecrosis, as acute chest pain is not uncommonly a precursor of myocardial infarction. And in this condition, the patient needs immediate cardiac care.
So, if you feel anxiety, panic, and fear of death when you're in pain, there's a 90% chance you've had a heart attack and you need to call an ambulance urgently. If you have a manometer, you will need to measure your blood pressure and count your pulse. When pulse slows to bradycardia (less than 50 beats/min) and blood pressure rises to 20–40 mm Hg for age, unstable angina should also be suspected and possibly transition to myocardial infarction. heart. .
You should not seek information on how to understand heart attack or osteonecrosis, it is much more effective to seek medical help. Even the most common electrocardiogram, done in a hospital emergency department, will show what's causing the pain syndrome: the heart or the spine. Independently, you can only rely on feeling when palpating. As a rule, with myocardial damage, palpation of vertebral processes does not give unpleasant sensations. But at the same time, there are clinical symptoms of osteonecrosis such as shortness of breath, feeling of lack of air, pallor of the skin, feeling of cold sweat sticking to the skin, cyanosis of the nasolabial triangle and severe muscle weakness. .
How to recognize lumbar bone necrosis?
Quite acute is the question of how to understand that osteonecrosis of the low back causes severe pain. Furthermore, with the defeat of some paired lenticular nerves, as well as plexus plexuses, clinical symptoms occur similar to diseases of the gastrointestinal tract and urinary system. These are constipation, diarrhea, frequent urination, etc. v.
How to understand that osteonecrosis of your back causes pain and all other clinical signs:
- no increase in body temperature;
- no nausea and vomiting;
- the tongue is not coated with white or yellow paint;
- when urinating, the color of urine does not differ from normal;
- when emptying the intestine, there is no straining and other painful sensations;
- There is no blood or mucus in the stool.
To exclude renal pathology, the Pasternatsky symptomatology test is performed. The patient stands with his back to the doctor. The doctor uses the palm of his hand to gently rub the lower edge of the dental arch. If pain is present, it is highly likely that low back pain is related to damage to the kidneys and ureters.
How to recognize lumbar bone tumor by indirect signs:
- with any movement, the pain increases sharply;
- Exacerbation that begins after severe exertion, heavy lifting, hypothermia, or overheating;
- stiff sensation of movements, often it is associated with muscle weakness;
- muscles in the lumbar region are strongly stretched, painful to palpation;
- pain may radiate along the path of the great nerves, for example, in the inguinal region, on the anterior abdominal wall, along the lower extremities;
- at rest, the pain syndrome quickly disappears.
When symptoms characteristic of osteonecrosis appear, it is important to contact a neurologist or chiropractor as soon as possible. Only an experienced doctor can rule out the possibility of vertebral deviation, herniated disc, spinal stenosis and other dangerous conditions that require immediate emergency care.
What to do with the pain of bone necrosis?
We have found a way to understand that pain arises from osteonecrosis. Right now, this is important information. You need to know how to behave properly and what to do to get rid of such a disease.
It is a degenerative degenerative disease of the cartilage tissue of the discs that does not go away on its own. This is due to a number of factors. First of all, calcification of the annulus surface results in loss of the ability to absorb fluid secreted by the working muscles. Second, in the process of reducing the height of the discs, there will be a secondary contraction of the ligaments and tendons. It will not be possible to restore the height of the intervertebral disc spaces needed to straighten the disc on its own.













































